Understanding Incompatibilities in IV Therapy: What Every Clinician Should Know
Intravenous (IV) therapy is a cornerstone of modern patient care, allowing for the rapid administration of fluids, medications, and nutrients. However, with its many benefits comes the critical need to understand incompatibilities—reactions that can compromise patient safety, drug efficacy, and clinical outcomes.
In our Basics of Peripheral IV Therapy course here at Pedagogy Education, we cover this topic in depth. But here’s a quick review for those looking to brush up on their knowledge or revisit the fundamentals.
What Are Incompatibilities?
Incompatibilities in IV therapy refer to undesirable reactions between medications, fluids, or both. These reactions are typically categorized into three types: physical, chemical, and therapeutic.
1. Physical Incompatibility
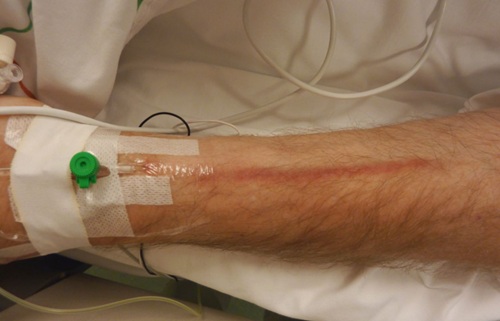
This is the most visibly obvious type. It usually results in:
- Precipitate formation
- Color change
- Cloudiness or haze
- Gas bubbles
These changes may look harmless but can lead to serious complications, such as embolism, myocardial damage, or harm to vital organs like the kidneys or liver.
2. Chemical Incompatibility
Unlike physical incompatibility, these reactions aren’t always visible. Chemical changes can alter:
- The molecular structure
- The pharmacologic properties of the drug
The result? Reduced potency or unexpected drug activity, which could mean the patient is receiving less (or more) of a drug than intended.
3. Therapeutic Incompatibility
This occurs when two or more drugs administered together (or closely together) interact in a way that:
- Diminishes their effectiveness
- Increases adverse effects
- Counteracts therapeutic intent
Understanding the pharmacodynamics of each medication is key to avoiding this type of incompatibility.
The Importance of Compatibility Checks
Before mixing or administering any IV solution, clinicians must:
- Verify compatibility using reliable reference sources (e.g., Trissel’s™ IV Compatibility)
- Assess drug stability and expiration dates
- Review the sequence of how medications are added
Solutions with insoluble matter or precipitates should never be administered due to the risk of emboli and organ damage.
What Affects Drug Stability?
Several factors influence how stable a medication remains once prepared:
- pH of the diluent
- Time the solution stands before use
- Presence of preservatives
- Light exposure (which can fuel chemical reactions)
- Concentration of the drug (degree of dilution)
- Temperature (some drugs need refrigeration)
- Order of mixing multiple medications
Even small deviations in these conditions can render a medication unsafe or ineffective.
Want to Learn More?
These are just the highlights. For a thorough understanding of IV therapy fundamentals—including compatibility and safety practices—be sure to check out our Basics of Peripheral IV Therapy course at Pedagogy Education. Whether you’re a new nurse or a seasoned professional, continuing education can be the difference between good practice and great practice.
Stay safe, stay informed—and never stop learning.
Explore the full Course Library here ➝ Course Library